Healthcare costs in the US have steadily risen for decades, accounting for $3.8 trillion or 17.7 percent of the country’s GDP. Because of this, one in five Americans skip or have skipped needed healthcare due to cost concerns—leading to a need for cost intervention.
With certain changes, telemedicine platforms can help reduce healthcare costs at a scalable level to accomplish significant cost savings for payers, providers, and patients alike.
The challenges with our current high-cost, low efficacy telemedicine system
Today’s telemedicine exhibits limited capacities—lacking the precise clinical examination necessary for long term adoption.
Integrating technology and connected devices to collect objective measurements, such as heart and lung sounds, into telemedicine platforms can help support better quality of care. However, further advancements are necessary to ensure that such integrations do not result in higher care costs.
Many of today’s telemedicine platforms represent significant cost for the clinicians using them. As a result, their use results in increased operating costs and overall healthcare costs. To truly lower costs, we need to replace the existing, expensive healthcare delivery system of today with a scalable, effective system that is easy to use—all in one integrated platform.
Improving ease of delivery by increasing accessibility through reduced patient-facing cost
Creating expensive technologies to replace our existing telemedicine platforms is not an answer for reducing costs. Instead, keeping the cost of telemedicine low enough to be scalable across patient populations is important in addressing the rising healthcare costs and making telemedicine a meaningful solution.
Currently, the connected devices required to ensure quality telemedicine visits typically cost upwards of $300, depending on the type of device. With many of these costs being patient-facing, the devices present unrealistic solutions in many households where individuals are unable or unwilling to purchase such an expensive device.
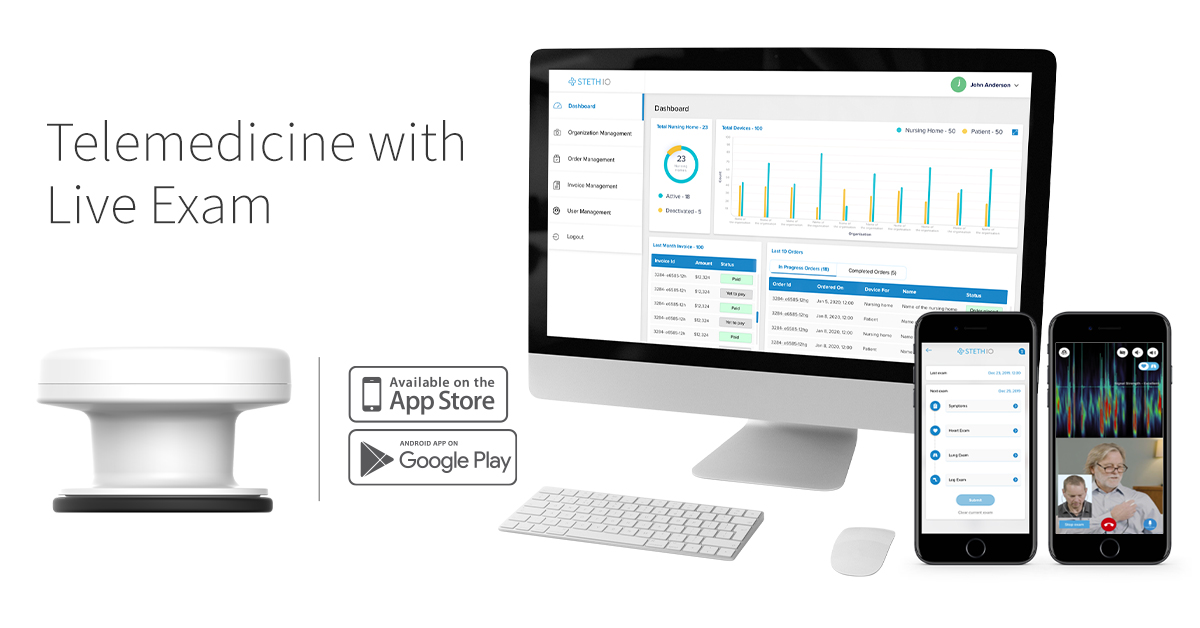
Increasing the accessibility of next-generation telemedicine platforms begins with making the technology and devices available, affordably. For example, Steth IO is a robust telemedicine platform that combines traditional audio-visual remote visits with a smartphone-compatible connected device that captures patient heart and lung sounds and generates visualizations of those sounds to highlight potential irregularities and problems. Despite its unique integrated telemedicine platform, the Steth IO platform provides significant cost savings compared to similar devices and platforms—making it a more viable and accessible solution for patients, their providers, and health plans.
Solutions like Steth IO that allow for meaningful telemedicine visits while keeping costs low ensure quality telemedicine is accessible for the general public and help fuel telemedicine expansion. As such, the devices become essential medical equipment to be kept at home—the same way many households keep a thermometer in their medicine cupboard. And unlike prescribed medications, connected devices do not have a shelf life making them an integral tool for years to come.
When we make the needed diagnostic devices more widely available, a paradigm shift occurs as telemedicine becomes an ongoing viable option for not only diagnosed patients with chronic conditions, but for those who may just need a clinician visit once or twice a year. Time and space shrink, giving more people access to care-–and clinicians the opportunity to see more patients with lower overhead.
Building affordable telemedicine at scale by reducing provider and payer overhead
Up until the pandemic, telemedicine provided a largely niche market, catering to those who were unable to leave the house or lived in remote areas that made visiting an in-person clinic difficult.
The next generation of telemedicine provides opportunities for all—including patients living next door to a clinic—to receive quality care without having to go into the clinic. With the right connected devices at home, patients can book an appointment, pay, and complete their visit all via their personal cell phone.
Bringing telemedicine out of a niche market and into a mass market significantly reduces care costs without compromising the quality of care. As more and more visits can be done effectively by telemedicine, providers are free to reduce spend on non-value-add expenses that are traditionally necessary in an in-person clinical setting. This could include reducing money spent on maintaining large clinic spaces and exam rooms, staffing reception desks and large teams of physician assistants, or even saving on smaller upfront costs like cleaning supplies and PPE. Over time, these changes result in across-the-board savings for payers, clinicians, and patients alike and an affordable long-term solution to reducing our high healthcare costs.
The cost savings associated with next generation telemedicine programs
The reduced costs that payers, clinicians, and patients see will ultimately pay for the cost of these technologies set up.
For payers, frameworks exist that reimburse payers for deploying these technologies into patient homes. As such, some payers opt to cover the cost of providing devices like blood pressure machines, or integrated telehealth platforms like the Steth IO that help ultimately reduce the cost of care on all fronts—including reducing high-cost utilization such as preventable ED utilization, inpatient admissions, and readmissions.
For clinicians, operational expenses are reduced as less money is needed to maintain, furnish, and staff a large brick-and-mortar clinic, resulting in lower overhead and significant savings. Patients also see savings as integrated telemedicine platforms allow them to stay connected with their physician—without incurring the cost of travel, childcare, or loss of pay that often accompany travel to a physical clinic.
As more integrated telehealth platforms continue to prove reduced costs—and maintain quality of care—our “next-generation telemedicine” ultimately becomes the next generation of healthcare.
Posted in News, telemedicine
