With 75.3M cases of COVID-19 as of February 1st, providers across the country are facing added difficulties in space, staffing, and triage as they struggle to adapt to the surges in infection caused by the Omicron variant.
Implementing solutions that address these challenges is not only important to ensuring continuity of patient care, but to reducing long-term care team burnout.
The difficulties faced as a result of Omicron
Since the start of the pandemic in February of 2020, 18 percent of healthcare workers have quit their jobs—and an additional 12 percent have been laid off—due to the stress of the pandemic, burnout, and insufficient pay.
With an already limited workforce, and rising numbers of healthcare workers becoming infected with the highly-contagious Omicron variant, many medical assistants and nurses today are being split between three or more providers. Not only does this increase risk of burnout, but it creates additional rooming shortages for taking needed patient vitals and work-ups prior to provider evaluations.
Telehealth can help alleviate these challenges—solving for space and staffing shortages and helping providers and health plans successfully navigate and counter surges in infection rates.
Adjusting to infection peaks with telemedicine
Telemedicine supports providers and patients during influxes in infections, like the Omicron variant, by bringing the care directly to a patient—reducing need for both clinical space and staff. For example, by facilitating at-home visits, clinics decrease the risk of infection from overcrowded waiting rooms and reduce the need for reception staff at the front desk.
Unfortunately, where traditional telemedicine solutions fall short is in being able to deliver clinically meaningful visits. Without the ability to take key vitals remotely, the quality of care providers are able to deliver is limited. Additionally, many of these platforms require significant cost and IT lift, causing additional administrative burden on already overwhelmed staff.
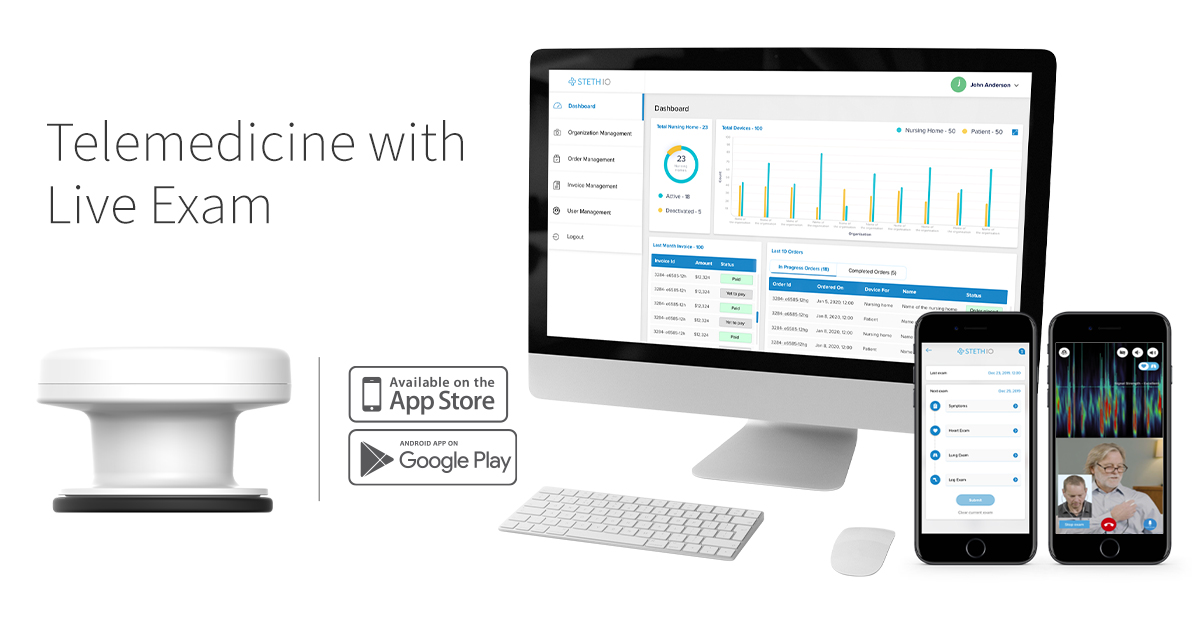
Steth IO supports providers in overcoming both the challenges brought upon by Omicron and the shortcomings of traditional telemedicine platforms through Telaspot: an intuitive platform offering remote vital monitoring.
Addressing the surges in Omicron with Steth IO
The Steth IO Telaspot delivers unique, innovative technology that facilitates remote patient examinations—not just remote visits.
With a stethoscope “Spot” device designed to work with existing patient smartphones, the Telaspot platform allows for remote examination of breathing, heart rate, and other vitals key to accurately diagnosing and triaging cases. By mimicking in-person clinical workflows, care teams are able to deliver meaningful remote care without having to relearn processes during stressful staff shortages. Furthermore, the platform can be implemented easily, requiring minimal IT lift, for seamless integration into both systems and workflow.
Such technology is especially useful for implementing hospital at home programs—allowing healthcare providers to both see and evaluate patients meaningfully during times of maximum capacity. With Omicron leaving more than half of states at or beyond 80% ICU capacity, solutions like Steth IO prove critical to reducing burdens on the acute healthcare system and addressing shortages of staff and space—all without sacrificing effective triaging.
A win for all
Ultimately, when we’re able to implement the right solutions, it’s a win for all involved.
With solutions like Steth IO, providers and care teams can benefit from reduced burden during times of pandemic and solve key challenges of space and rooming. Health plans benefit as members are able to receive appropriate triaging from symptom onset—reducing unnecessary high-cost utilization and facility crowding. Finally, patients win as they’re able to receive care at home—eliminating risk of exposure during travel to appointments or while waiting in overcrowded clinics or emergency departments—without compromising their quality of care.