What COVID-19 regulations have lead to the progression of the telemedicine movement, and how we can ensure that telehealth continues to grow
The COVID-19 pandemic resulted in a complete disruption of our healthcare system. As infection risk grew, news reports of hospitals unable to accommodate the growing number of COVID patients were widespread.
In reality, the very early days of the pandemic looked different. According to a study published by the National Syndromic Surveillance Program, ED visits in March and April of 2020 were down 42 percent, and additional surveys found that in-clinic visits dropped to 20-30 percent of their usual volume.
Why? The emergence of telehealth.
The progression of telemedicine as a result of COVID-19
COVID-19 fueled rapid development and adoption of quality telemedicine solutions to provide a broader range of health services.
In March 2020, telemedicine visits rose by over 1000 percent year over year as both patients and providers moved to quick adoption of telehealth. Since then, use of telemedicine has remained high—even outside peak periods of COVID-19. This achievement, completed in months, would normally take a decade to accomplish and would be impossible without the recent changes in healthcare regulations.
CMS changes impacting telemedicine during the COVID-19 pandemic
CMS restrictions previously barred widespread telehealth use in many Medicare and Medicaid populations. The COVID-19 pandemic led to a shift in these regulations, with CMS allowing telehealth visits to be originated from a patient’s home and be reimbursed at the same rate as an in-person visit.
These shifts allowed patients living in rural and urban communities the same access to telehealth and made telemedicine a financially viable choice for providers through parity of payment.
Additional administrative changes were made outside the CMS scope that furthered the growth of telemedicine. These included the removal of cross-state restrictions on medical licenses for telemedicine visits and a relaxation of HIPAA regulations to facilitate information sharing across providers for improved continuity of care.
The results of change: Improved care at reduced costs
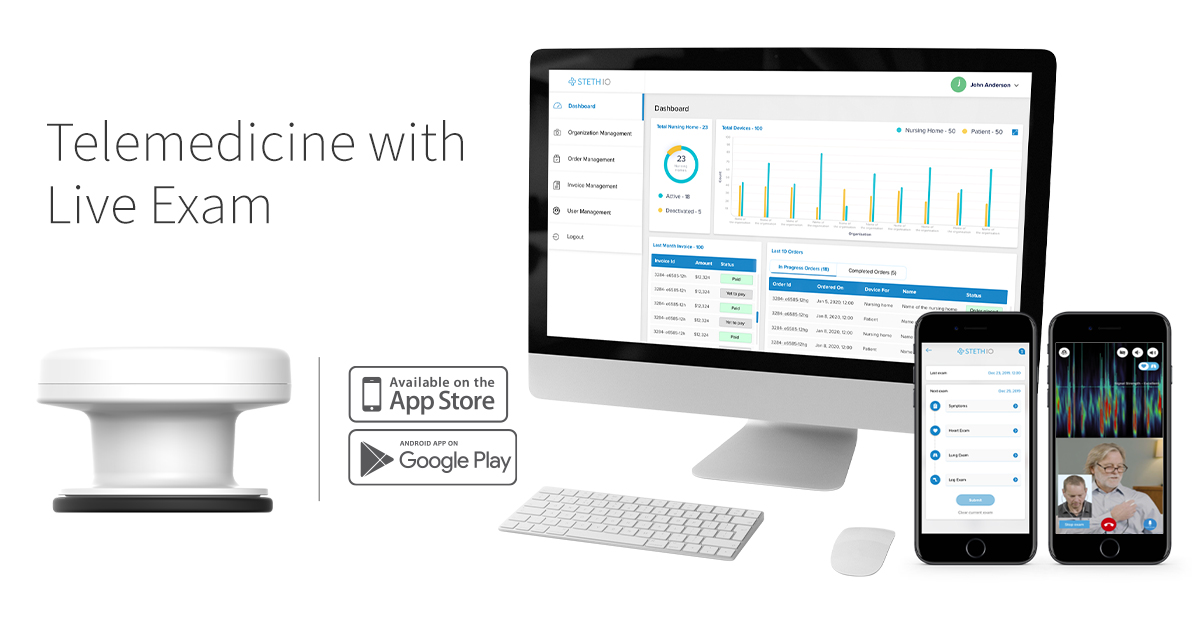
The current pandemic serves as a pilot for telehealth, ultimately proving that remote care brings numerous benefits—including improved cost and quality of care. This is especially true for telehealth platforms like Steth IO that rival in-person visits by offering full remote examination capabilities in addition to traditional telemedicine audiovisual functionality.
In addition, telemedicine surpasses in-person care with its ability to provide timely access to care. Patients who struggle to get in and see a provider due to limited exam rooms and appointments—or personal inability to take time off work, travel, or find childcare—can receive needed care when and where they need it, reducing the risk of condition exacerbation and high-cost utilization.
Reducing costs of care through telemedicine
Insurers and providers are reducing costs with the minimal overhead required for digital and remote health visits. Currently, 88 percent of studies show that telemedicine is an effective tool for achieving meaningful cost savings compared to conventional lines of care.
But even this decrease in overhead is minimal to the long-term cost savings both insurers and patients will see as patients are more effectively triaged—reducing the need for walk-in clinics as well as high-cost ED utilization and readmissions. When the cost of technology implementation is covered through government grants or funding from innovative programs like VBID, those savings are even more significant.
Continuing to improve healthcare post-pandemic through telemedicine
Telehealth is here to stay, but its strength and reach will depend on maintaining a number of the regulations and “wins” that facilitate its current widespread use. With the right policies in place, telehealth can be the default system of care—guaranteeing better access to healthcare across populations and ensuring infrastructures are in place to provide consistent, quality care, even in the event of another public health crisis.
Improving and maintaining beneficial telehealth policies post-covid
The relaxed HIPAA regulations will ultimately need to return to their former stringencies, but other regulations created for telehealth mid-pandemic should be considered for long-term adoption as we move forward.
For example, robust telemedicine platforms with diagnostic capabilities like that provided by Steth IO and its Spot device have proven to be an acceptable match for in-person care and should be billed and reimbursed as such. Code classifications may differ, but ultimately telehealth payments need to remain reimbursable in parity with traditional clinic visits.
In addition, the medical licensure restrictions across state lines may go back into effect, but we now have goals that we can strive for in seeking out a national healthcare telehealth license or increased reciprocity between state licenses for telehealth.
Telehealth as the new normal
The U.S. is well-positioned to make all healthcare visits, by default, a remote healthcare visit. Even now, roughly 70 percent of clinical visits taking place—both in primary care and in many specialties—could already be taking place effectively with telemedicine.
Using the innovation momentum gathered from the current pandemic to create long term change in how insurers and providers think about, utilize, and advocate for telemedicine—both within the healthcare system and through patient outreach—can open doors for a quality and cost-effective solution for addressing, diagnosing, and treating many conditions. This ultimately strengthens our health system, reduces the cost of care, increases the quality of care, and improves the access for care across populations for better overall health outcomes.